We are dedicated to protecting the health, safety, and well-being of children and families. Below are resources to support you and your family during the COVID-19 pandemic.
For the latest information on COVID-19, please visit the Minnesota Department of Health website or call the MDH COVID-19 hotlines between 7 a.m. to 7 p.m. (interpreters available).
• Health questions: 651-201-3920 or 1-800-657-3903
• Schools and child-care questions: 651-297-1304 or 1-800-657-3504
Supporting Mental Well-being During COVID-19
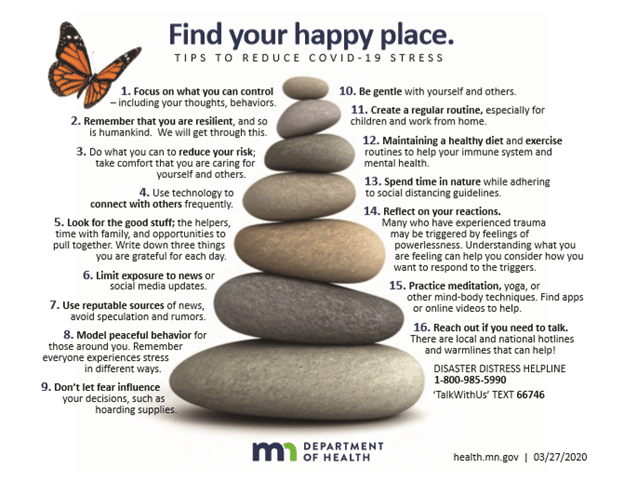
It’s normal to be experiencing increased stress and anxiety right now. It is important to be gentle with yourself and others, and to take steps to support both your own and your family’s mental well-being. Consider these tips to support your mental well-being during the COVID-19 response.
Managing Stress and the Threat of COVID-19
While it is critical during this time to take care of your physical health, you also need to pay attention to your emotional and mental health. Recognize and monitor your stress levels during the COVID-19 pandemic.
- Physical Reactions:
- You may experience low energy, exhaustion, sleep problems, headaches, muscle aches, appetite change, increased heart rate, or upset stomach.
- Emotional Reactions:
- You may experience anxiety, worry, fear, sadness, tearfulness, and/or loss of interest in usual enjoyable activities. You may also feel frustration, irritability, anger, or helplessness. Strong feelings that won’t go away, last longer than a few weeks or are interfering with normal functioning may be symptom(s) of depression or anxiety and are a sign that you should seek professional mental health help.
- Behavioral Reactions:
- Some behaviors triggered by stressful events need to be stopped because they can not only harm your physical and mental health but they also make the situation worse for others. Harmful behaviors include, but are not limited to, increased dependence on nicotine or alcohol, substance abuse, gambling, bullying, blaming others, spreading rumors or conspiracy theories and ignoring public health and safety recommendations.
- Cognitive Reactions:
- The stress of COVID-19 may affect your ability to think clearly, make it harder to pay attention, solve problems, or remember. It does not mean that you are “crazy” or “losing your mind.” These are common reactions in times of high stress. They are signals to you to take action to care for yourself.
Psychological First Aid (PFA) Strategies
While physical First Aid is used to reduce physical pain from a body injury, Psychological First Aid (PFA) is a strategy to reduce the painful range of emotions and responses experiences by people exposed to high stress situations. The PFA strategies provided below will help you to reduce stress in yourself, and others.
- Safety
- Practice basic cold and flu precautions by washing your hands thoroughly with soap and water, covering your cough, and staying home when you are sick. Follow COVID-19 specific health and safety guidance provided by Lower Sioux EOC and Minnesota Department of Health. When following the recommendations of trusted health professionals, fear, stress and misinformation is reduced and community safety enhanced.
- Calm
- Maintain your day-to-day normal activities and routine where possible. Eat healthy, exercise, avoid nicotine, alcohol and illegal drugs, cool your temper, do things that bring you joy and laughter, and try to get enough sleep. Learn and practice coping techniques such as deep breathing, visualizations, and muscle relaxation.
- Connect
- Stress is reduced during a crisis when we can connect with our friends and loved ones. Maintaining connections with supportive family and friends can bring a sense of comfort and stability. Talking through our concerns, thoughts, and feelings with others can also help us find helpful ways of thinking about or dealing with a stressful situation. Consider creating a disaster communication plan so that you are able to connect with loved ones and support services during crises.
- Culturally relevant communication emergency plans for families and households are available at https://www.ready.gov/indian-country and https://www.ready.gov/sites/default/files/2020-03/create-your-family-emergency-communication-plan.pdf
- Empowerment and Self-Efficacy
- You can reduce your stress by taking positive steps to protect yourself and your loved ones. Control your exposure to news and social media reports about COVID-19. While it is important to stay aware of the situation, overexposure will keep you in a heightened state of stress. Instead, focus your attention on things that are positive in your life and take action over the things you do have control over. Develop a COVID-19 disaster kit so that you will have the supplies you need if you or a family member gets ill.
Parent/Caregiver Guide to Helping Families Cope with COVID-19
Information about COVID-19 is rapidly evolving as new details are confirmed and new questions emerge daily. In the event of an outbreak in your community, as a parent/caregiver, your first concern is about how to protect and take care of your children and family. Knowing important information about the outbreak and learning how to be prepared can reduce your stress and help calm likely anxieties.
What You Should Know
- Coronaviruses are a large family of viruses that cause illness ranging from the common cold to more severe diseases. COVID-19 is caused by a novel coronavirus; this means it is a new strain that has not been previously identified in humans.
- COVID-19 is a respiratory disease that is mainly spread person-to-person. Currently, there is no available vaccine or curative treatment, so the best preventative strategy is to avoid exposure.
- So far, children appear to be much less affected by COVID-19, which was also seen after other coronavirus outbreaks.
- Children with pre-existing illnesses may have different risk levels, so you should discuss with your child’s medical team.
- To reduce the spread of the virus, a variety of approaches will be used, including keeping those who are sick away from others and promoting healthy hygiene strategies. Additional recommendations for ways to contain the virus could include canceling of events that attract large numbers of people; closing schools, public transit or business; and required quarantine, which is the separation and restriction of movement of people who might have been exposed to the virus.
Preparing your Family for a Potential Infectious Disease Outbreak
- Information and Communication
- Identify how you will keep up with rapidly changing information on COVID-19.
- In rapidly changing health events and outbreaks such as COVID-19, there can be large amounts of incorrect or partially correct information that can add to stress and confusion as a parent/caregiver. Identify a few trusted sources of health information.
- CDC: https://www.cdc.gov/coronavirus/2019-ncov/index.html
- Information on children and COVID 2019:
- https://healthychildren.org/english/health-issues/conditions/chest-lungs/pages/2019-novel-coronavirus.aspx
- Reducing Your Family’s Risk: Hygiene, Medical Care & Supplies
- Have all family members practice preventive behaviors including:
- Vigilant 20 second hand washing with soap and warm water (length of ABC song) or use alcohol based hand sanitizer that contains at least 60% alcohol.
- Avoiding close contact with people who are sick.
- Staying home when sick.
- Covering mouth and nose when coughing or sneezing.
- Keep basic health supplies and regular medications on hand.
- If your child takes medication for a chronic condition, talk with your child’s medical provider about plans to get a supply at home that will last through any period of at home isolation for your family.
- Find ways to encourage proper hygiene and health promoting behavior with your children (create drawings to remember family routines; sing a song for length needed to wash hands like the A-B-C or Happy Birthday song, twice). Include them in household jobs or activities so they feel a sense of accomplishment. Provide praise and encouragement for engaging in household jobs and good hygiene.
Self-Care and Coping
- Modify your daily activities to meet the current reality of the situation and focus on what you can accomplish.
- Remember, you are a role model for your children. How you handle this stressful situation can affect how your children manage their worries.
Helping Children Cope with Changes Resulting from COVID-19
- Your child may respond differently to an outbreak depending on their age. Below are some reactions according to age group and best ways to respond:
| AGE GROUP | REACTIONS | HOW TO HELP |
| INFANTS AND TODDLERS (ages 0-2) | Cannot understand that something bad in the world is happening but they know when their caregiver is upset. They may cry, and withdraw from people/toys. | As a caregiver, try to remain calm and as stress free as possible. Practice deep breathing strategies to calm down. Keep normal routines and provide a lot of emotional and verbal support. |
| PRESCHOOL (ages 3-5) | Fear of being alone, speech difficulties, loss of bladder/bowel control, constipation, bed-wetting, change in appetite, increase in tantrums, whining or clingy behaviors. | Patience and tolerance, provide reassurance (verbal and physical), encourage expression through play, plan calming, comforting activities before bed, maintain regular family routines. |
| SCHOOL-AGE (ages 6-12) | Irritability, whining, aggressive behavior, clinging, nightmares, sleep/appetite disturbance, head/stomach aches, forgetfulness about chores and new information learned at school. | Patience, tolerance, & reassurance, engaging educational activities, physical activities and exercise, structured household chores and routines, encourage expression through plan and conversation. |
| ADOLESCENT (ages 13-18) | Headaches, sleep/appetite disturbance, agitation or decrease in energy, apathy, isolating from peers and loved ones, avoiding schoolwork. | Encourage continuation of routines, encourage staying in touch with friends through internet, limit media exposure, discuss and address stigma and potential injustices occurring during outbreak. |
- Be aware of how you talk about COVID-19. Your discussion about COVID-19 can increase or decrease your child’s fear. If true, remind your child that your family is healthy and you going to do everything you can to keep loved ones safe and well. Carefully listen or have them draw or write out their thoughts and feelings and respond with truth and reassurance.
- Demonstrate deep breathing. Deep breathing is a valuable tool for calming the nervous system. Do breathing exercises with your children and on your own.
- Focus on the positive. Celebrate having more time to spend together as a family. Make it as fun as possible. Do family projects, organize belongings, create masterpieces. Sing, laugh and go outside, if possible, to connect with nature and get active! ????
- Establish and maintain a daily routine. Keeping a regular schedule provides a sense of control, predictability, calm and well-being. It also helps children and other family members respect others’ need for quiet or uninterrupted time.
- Offer lots of love and affection.
- Most children will manage well with the support of parents and other family members, even if showing signs of some anxiety or concerns, such as difficulty sleeping or concentrating. Parents and caregivers should contact a professional if children exhibit significant changes in behavior or any of the listed symptoms for more than 2 weeks.
Seeking Additional Help
What Helps:
- Talk with and listen to others
- Do things that help you relax:
- Breathe deeply
- Listen to music
- Do things you enjoy like sports, hobbies, reading
- Move your body, exercise
- Eat healthy
- Get enough sleep
- Try to keep a normal schedule
- Learn what things stress you out
- Check in on friends and family
- Focus on what you can do instead of what you cannot do
- Take breaks from the news and social media
What Does NOT help:
- Smoking, drinking, or using drugs more than you should
- Avoiding thinking or talking about the event
- Avoiding family, friends, or activities
- Watching a lot of TV, and social media
- Playing a lot of computer or video games
- Doing risky things like driving dangerously or abusing substances
Signs of Stress Related to a Crisis
- Sleeping or eating problems
- Pulling away from people & events
- Having very little or no energy
- Feeling sore or in pain
- Feeling sad, numb, helpless, hopeless, confused, forgetful, angry, upset, worried, or scared.
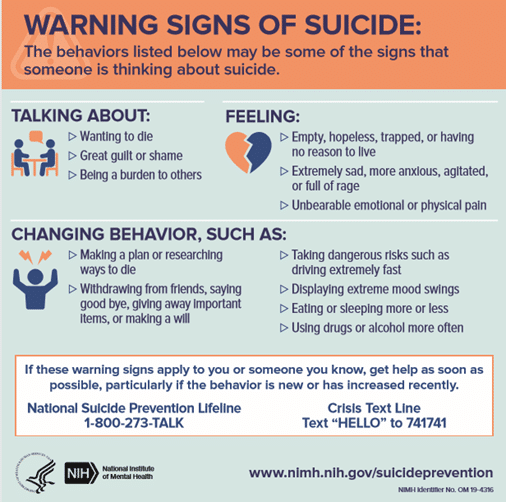
Warning Signs: Get Help Now!
If you, or someone you know, is talking about harming themselves or others, get help now!
Contact the Disaster Distress Helpline (1-800-985-5990). Danger signs include:
- Thinking of hurting or killing yourself or someone else
- Saying things like wanting to “end it all” or “go to sleep and never wake up again”
- Giving away possessions
- Unable to perform daily tasks
- Excessive anger
- Yelling or fighting with family or friends
- Driving under the influence
- Using drugs
Community Resources
Jay Hunter, LMFT, (651) 269-0485 (15-20-minute calls at no cost to our community)
Rose Joiner, LMFT, (612) 406-2224 (15-20-minute calls at no cost to our community)
Tuesday & Thursday Support Meetings (AA/NA/Circle) will be available over the phone from 12PM – 1PM. Please call 507-697-8679 and you will be added to call automatically. These meetings are chaired by Woniya Kini Staff Members.
Western Mental Health Center Mobile Crisis at (800) 658-2429
Sojourn Counseling at 507-430-0261 currently offering counseling group in response to COVID- 19. Call for more details. There is no cost to individuals.
Domestic Violence
Are Domestic Violence, Sexual Assault, and Stalking services still available?
Yes! We are still here for you. Please call any number below at any time of the day to let us know how we can help you end the cycle of abuse. You will be connected to the services you need, and we will keep everything we do and say completely confidential.
If you experience any of the following definitions of abuse, please call.
Domestic violence can be defined as a pattern of behavior in any relationship that is used to gain or maintain power and control over an intimate partner. Sexual Assault occurs without explicit consent of the victim. Stalking is any repeated and unwanted contact (physical presence or cyber stalking) that makes you feel unsafe.
Lower Sioux Victim Services:
Minnesota Indigenous Woman Society (MIWS): 507-624-HELP (4357)
MIWS Crisis line – Beth O’Keefe 507-627-4357
Lower Sioux Police Department: 507-430-1622 or 911; or 320-522-0216
Women Victims Services Coordinator: 320-522-0216 (ask for Kim H.)
Hotlines
Mental health hotlines provide free support to support Minnesotans experiencing mental distress are listed below. Please also consider contacting the National Alliance on Mental Illness (NAMI) Minnesota (1-888-NAMI-Helps / 1-888-626-4435) or the Minnesota Association for Children’s Mental Health at (800-528-4511) to connect for help, to navigate the mental health system, for support and for resources.
• Crisis Text Line: The 24/7 emergency service is available if you or someone you know is experiencing a psychiatric or mental health crisis.
- Text MN to 741741
• Redwood County Crisis Contacts
- Adult Mental Health Crisis Response Number – 1-800-658-2429
- Children Mental Health Crisis Response Number – 1-800-658-2429
• Minnesota Warmline: If you an adult needing support: Talk to a specialist who has firsthand experience living with a mental health condition.
- Call 651-288-0400 or text “Support” to 85511
• National Suicide Prevention Lifeline: The 24/7 lifeline provides support when in distress, has prevention and crisis resources for you or your loved ones, and resources for professionals.
- Call 1-800-273-TALK (8255)
• Substance Abuse and Mental Health Services Administration Disaster Distress Helpline: Offers crisis counseling and support if you or a family member is experiencing emotional distress related to a disaster.
o Call: 1-800-985-5990
